The Diabetes Epidemic: What we need to understand about the basic physiology of Type 2 Diabetes [article]
Why is Type 2 Diabetes such a problem?
Type 2 Diabetes is one of the biggest international health challenges in the world. The number of people in New Zealand with Type 2 Diabetes has doubled in the last 10 years, although the true extent of the disease remains unknown. It is estimated that for as many individuals that are diagnosed with Type 2 Diabetes, there is the same amount of people living with the disease who don’t even realise that they have it! The complications associated with Diabetes – for example hypertension, heart disease, and kidney problems – cost countries billions each year in health care, and can shorten a person’s life expectancy by up to 12 years.
How does someone get Type 2 Diabetes?
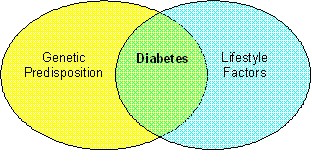
Previously it was believed that Type 1 Diabetes was more of a ‘genetic’ disease, and Type 2 Diabetes developed because of unhealthy lifestyle factors – poor nutrition, inactivity and excess body fat (especially abdominal fat). However studies on identical twins have shown that there is a stronger genetic link in Type 2 Diabetes than Type 1. The unhealthy lifestyle factors act more like a ‘trigger’.
A combination of a genetic pre-disposition and lifestyle risk factors can lead to Type 2 Diabetes developing.
What is the physiology of Type 2 Diabetes?
The physiology of Type 2 Diabetes is not 100% understood and is constantly being researched. There are many possible factors that could contribute to problems with glucose control in our bodies. What we do know about the physiology of Type 2 Diabetes is that it is caused by a combination of the following:
1. The body’s cells (especially skeletal muscle) may be resistant to the action of insulin. This is called peripheral insulin resistance. Remember insulin acts like a ‘key’ to ‘unlock’ the cell and let the glucose in. With insulin resistance it’s almost like somebody has changed the locks to our cells –the key no longer works!
2. Insulin may not be produced or released quickly enough when we eat. This is called impaired glucose tolerance (IGT), and happens when there is a problem with the function of the insulin-producing cells (the beta cells) on the pancreas.
3. The body may not be making enough insulin – again due to some kind of problem with or damage to the beta cells.
The pancreas does initially produce insulin with Type 2 Diabetes, but as insulin resistance develops and blood glucose levels rise, the pancreas steps up its production to try to lower those glucose levels. The pancreas doesn’t know that the cells are resistant to the insulin, it just knows it needs to get those glucose levels down! Eventually the pancreas appears to ‘wear itself out’, and insulin production begins to decline. If glucose levels remain uncontrolled over a period of time, Type 2 Diabetics may find that they require insulin injections to bring their glucose levels down.
Some of the latest research suggests that by the time insulin resistance is diagnosed, there will already be some problem with insulin production and/or release. This means that many Type 2 Diabetics will end up needing insulin injections.
What are the symptoms of Type 2 Diabetes?
The most common symptoms are similar to Type 1 Diabetes - excessive urination, excessive thirst and fatigue. When fasting glucose levels (i.e. not eating overnight before a blood test) reach over 7mmol/L, and the symptoms of Diabetes are present, Diabetes is diagnosed. If the cause of the high glucose levels is insulin resistance, the insulin levels in the blood will also be high.
Can you cure Type 2 Diabetes?
There is no ‘cure’ for Type 2 Diabetes, so treatment focuses on managing the disease to prevent longer term complications. This generally involves encouraging the individual to make healthy lifestyle changes. Excess body fat is closely linked with Type 2 Diabetes – 90% of individuals diagnosed are overweight or obese. Weight loss is a common management goal, achieved through decreasing calorie intake (especially fatty and sugary foods) and increasing physical activity levels.
Exercise is particularly important in the management of Type 2 Diabetes, as it has been shown to increase the transport of glucose into skeletal muscle cells, and increase insulin sensitivity. This makes it a valuable tool in helping maintain glucose levels in a safe range – which is critical in preventing those long term complications. Remember high glucose levels can damage the blood vessels in the body, leading to many different complications e.g. hypertension, and kidney, eye and foot problems.
Are there any risks with exercise?
Upon diagnosis of Type 2 Diabetes, glucose lowering medication is often prescribed. Some but not all of the different medications for Type 2 Diabetes pose a risk of hypoglycaemia when exercising. As fitness professionals we must find out the name of all the medications our client is taking – and with Type 2 Diabetes there may be a few! It is a good idea to talk to your client and their doctor and see whether adjustments in medication or carbohydrate intake need to be made before or after an exercise session.
There may be other risk factors present in your client with Type 2 Diabetes – including high blood pressure, high cholesterol, or any other illnesses associated with an unhealthy lifestyle.
Initial aims when training a type 2 Diabetic client
The biggest challenge in training a client with Type 2 Diabetes is often helping them to change their behaviour. They may have many barriers to exercise and healthy eating, and their physical capabilities – especially if complications or other health conditions are present – may be limited. Medical clearance from the doctor is mandatory before your client begins their exercise program, and you may find that you need to prescribe short duration, low intensity exercise when starting out. We may know that our client needs to work harder and longer to achieve their weight loss and fitness goals, but our initial focus should be on safety promotion and program adherence.
